Neurology:偏头痛,偏头痛残疾,创伤和性别少数群体个体的歧视
2022-09-02 Naomi MedSci原创
近日,一项发表在Neurology上的研究发现,偏头痛在性和/或性别少数(SGM)成年人样本中很常见。既往创伤和歧视经历与偏头痛残疾增加有关。精神病合并症在这种关系中发挥重要作用。
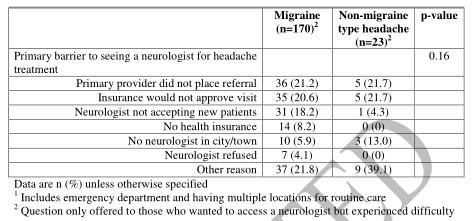
近日,一项发表在Neurology上的研究试图描述,在性和/或性别少数(SGM)成年人样本中,偏头痛的频率和严重程度,并检查创伤、歧视和偏头痛相关残疾之间的关系。
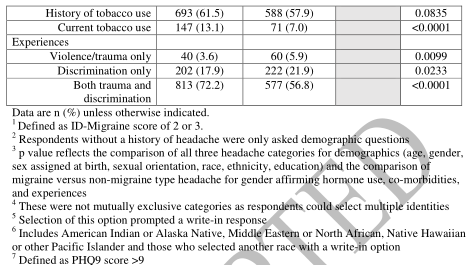
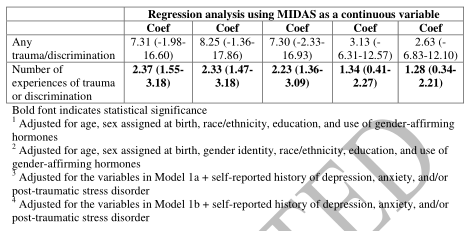
研究人员在2018年8月至10月的“身份和平等差异的人口研究”中对 SGM 人群进行了横向研究研究。主要的暴露是任何创伤或歧视,不管归因。根据偏头痛残疾评估(MIDAS)问卷评分≥11,主要结果为中重度偏头痛残疾。研究人员还进行了描述性分析,将有偏头痛的受访者与没有偏头痛的受访者进行比较。多变量 Logit模型研究了创伤/歧视和偏头痛残疾之间的关系,首先控制了社会人口学和临床因素,然后控制了精神病合并症。
结果:
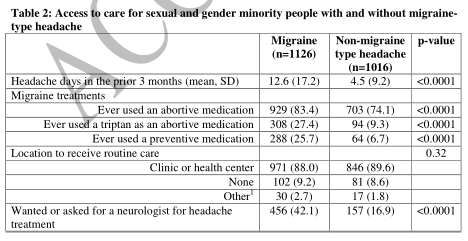
- 在3325名受访者中,1126名(33.9%)通过 ID-偏头痛标准筛选出偏头痛阳性。大多数偏头痛患者自我报告中度(n = 768,68.2%)或严重(n = 253,22.5%)强度。
- MIDAS 评分中位数为11(四分差[ IQR ]5-25)。大多数偏头痛患者(n = 1055,93.7%)报告有创伤或歧视史。
- 在未经调整的分析中,暴露于创伤和歧视与较高的中重度残疾几率相关(OR 1.76,95% CI 1.34-2.32)。
- 在调整了自我报告的焦虑、抑郁和创伤后心理压力紧张综合症的精神病合并症后,这种关联失去了统计学意义。
结论: 偏头痛在该SGM 成年人样本中很常见,以前的创伤和歧视经历与偏头痛残疾增加有关。该研究结果表明,精神病合并症在这种关系中发挥重要作用,确定了SGM 患者偏头痛残疾的一个潜在的可改变的危险因素。 。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言























#群体#
160 举报
#Neurol#
145 举报
#创伤#
219 举报
#歧视#
130 举报
讲的真好,很受益
134 举报
签到学习
115 举报
好文章,值得一读。
141 举报