拥有84%的5年生存率,美国治疗子宫内膜癌的“武器”是精准手术和合理用药!
2022-09-06 厚朴方舟 网络
子宫内膜癌,即子宫癌,2020年子宫内膜癌新发癌症42万,在女性常见肿瘤中排行第六,是常见的妇科恶性肿瘤。但值得庆幸的是,与其他恶性肿瘤相比,子宫内膜癌的预后效果较好。
子宫内膜癌,即子宫癌,2020年子宫内膜癌新发癌症42万,在女性常见肿瘤中排行第六,是常见的妇科恶性肿瘤。但值得庆幸的是,与其他恶性肿瘤相比,子宫内膜癌的预后效果较好。目前,美国子宫内膜癌总体5年生存率84%,成为了子宫内膜癌患者治疗的优选。那么,美国是如何治疗子宫内膜癌的呢?
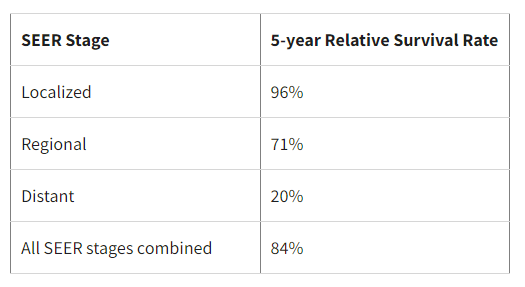
▲美国子宫内膜癌5年生存率数据
01手术治疗
手术是子宫内膜癌治疗的主要方案,即使是晚期子宫内膜癌也可以通过手术获益。
临床治疗时,可以根据肿瘤的侵袭程度选择手术方案,如果肿瘤尚未扩散到子宫外,通过采用子宫切除术联合双侧输卵管卵巢切除术(BSO)根治肿瘤,术中多采用淋巴结切除术确定癌症是否转移;如果子宫内膜癌已经进展到晚期,通过子宫切除术也可以有效改善患者的预后。
近年来,随着微创技术的发展,腹腔镜手术和达芬奇机器人手术在子宫内膜癌手术治疗领域的应用越来越广泛。相比传统的开腹手术,腹腔镜手术和达芬奇机器人手术伤口更小,并发症更少。
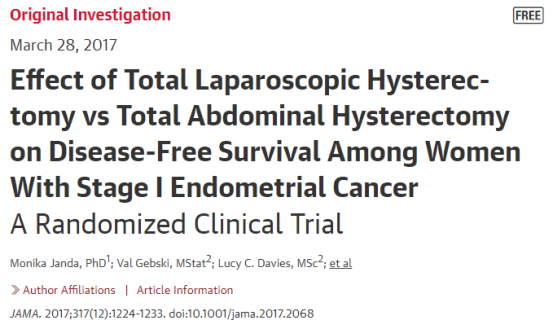
2017年发表的一项研究纳入了 760 名早期子宫内膜癌患者,评估了腹腔镜全子宫切除术与开腹全子宫切除术的有效性和安全性。研究结果显示,采用腹腔镜全子宫切除术与开腹全子宫切除术后的无病生存率相似,腹腔镜全子宫切除术的 4.5 年无病生存率为 81.6%,开腹全子宫切除术为81.3%;但是采用腹腔镜手术治疗子宫内膜癌的术后不良事件发生率更低[2]。
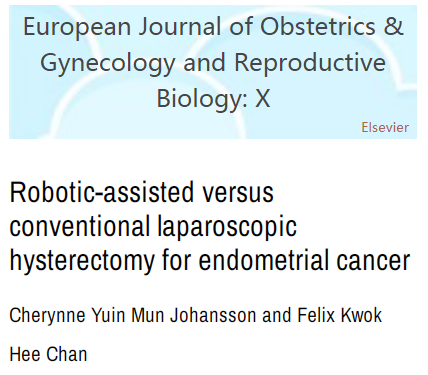
2020年的另一项研究评估了全腹腔镜子宫切除术 (TLH)与机器人辅助腹腔镜子宫切除术 (RALH) 用于子宫内膜癌治疗的效果。研究结果显示,与全腹腔镜子宫切除术相比,机器人辅助腹腔镜子宫切除术治疗子宫内膜癌的术后并发症发病率更低、失血量更少(78 mL vs 22 mL)、住院时间更短(1.8天 vs 1.2天)。
但是,需要注意的是,无论是达芬奇机器人手术、腹腔镜手术还是开腹手术,都需要经验丰富的外科医生进行,经验丰富的医生对手术的细节感知较深,可以预知到手术的危险性、手术中可能出现的问题,从而提前预防,在提高手术成功率的同时,降低手术对患者造成的伤害。
02靶向及免疫治疗
晚期子宫内膜癌常通过化疗、激素治疗、靶向治疗以及免疫治疗等药物治疗来延长生存期。其中,靶向治疗和免疫治疗的出现为许多晚期子宫内膜癌患者带来了新的生存机会。
目前Lenvatinib(Lenvima)、贝伐单抗、mTOR抑制剂——Everolimus(Afinitor)与Temsirolimus(Torisel)、PD-1抑制剂Pembrolizumab (Keytruda) 和 dostarlimab (Jemperli)等创新疗法均已被FDA批准用于子宫内膜癌的治疗,显著延长了晚期子宫内膜癌的生存期。
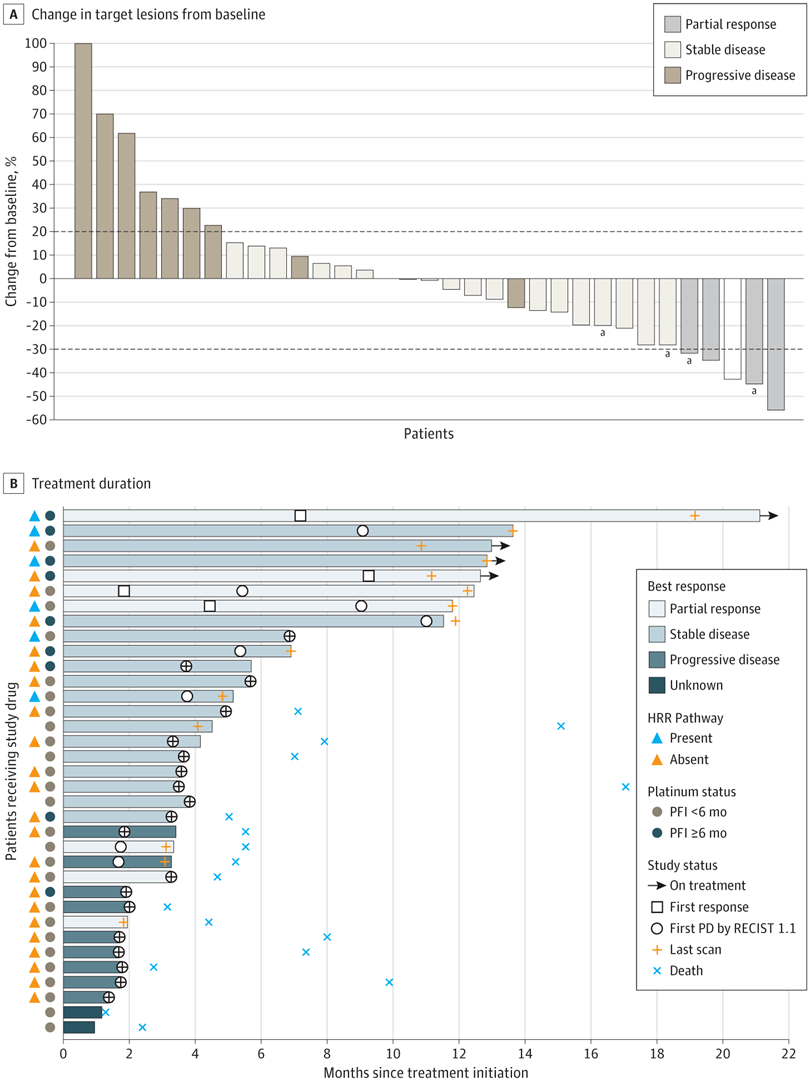
除此之外,免疫+靶向的联合疗法也为子宫内膜癌的治疗带来了新的选择。
2021年7月,美国FDA已完全批准抗PD-1疗法Keytruda,联合口服多受体酪氨酸激酶抑制剂Lenvima,用于治疗既往在任何情况下接受系统治疗后疾病进展、不适合根治性手术或放疗、经检测证实不是微卫星高不稳定性(MSI-H)或不是错配修复缺陷(dMMR)的晚期子宫内膜癌(EC)患者。

今年1月,《新英格兰医学杂志》公布的研究结果显示,与化疗组相比,Keytruda+Lenvima的组合疗法显著延长了晚期子宫内膜癌患者的生存期。具体数据为,在所有患者中,Keytruda+Lenvima组的中位总生存期为18.3个月,化疗组仅为11.4个月;中位无进展生存期为7.2个月,化疗组仅为3.8个月;在表现为低频度微卫星不稳定(MSI-L)或微卫星稳定(MS-S)的人群(pMMR)中,Keytruda+Lenvima组的中位总生存期为17.4个月,化疗组仅为12个月;中位无进展生存期为6.6个月,化疗组仅为3.8个月。

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#精准手术#
101 举报
#内膜#
100 举报
认真学习了
85 举报
#生存率#
0 举报
#合理用药#
108 举报
#精准#
113 举报