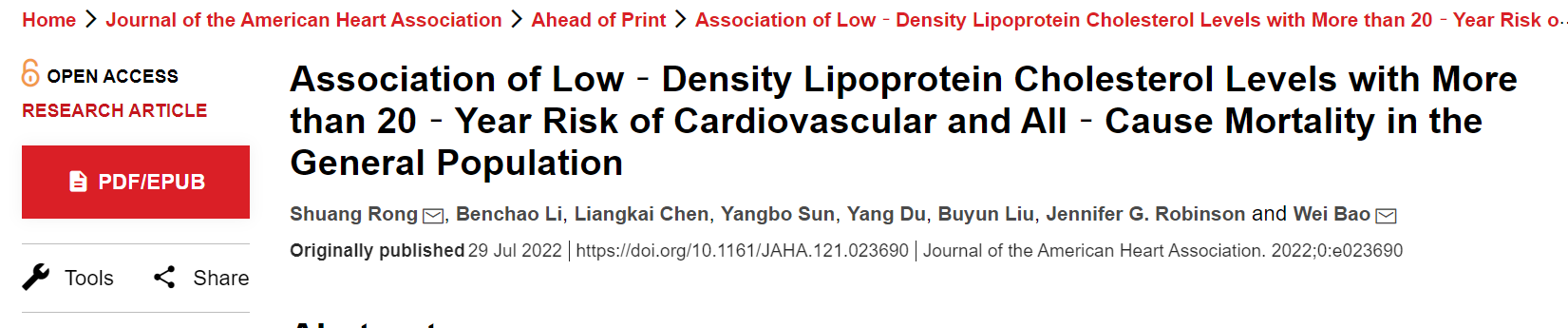
JAHA:低密度脂蛋白胆固醇水平与心血管和全因死亡风险之间的关系
2022-08-01 MedSci原创 MedSci原创
非常低和非常高的LDL-C水平都与心血管疾病死亡风险增加有关。极低的LDL-C水平也与全因死亡率和卒中死亡的高风险相关。需要进一步调查以阐明一般人群中CVD健康的LDL-C水平的最佳范围。
当前的胆固醇威廉亚洲博彩公司 已为心血管疾病(CVD)高危人群推荐了极低的低密度脂蛋白胆固醇(LDL-C)治疗目标。然而,最近的观察性研究表明,极低的LDL-C水平可能与死亡率增加和其他不良结局有关。在美国普通人群中,LDL-C水平与总体和心血管死亡的长期风险之间的关联仍有待进一步研究。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在这项前瞻性队列研究中纳入了14035名年龄在18 岁或以上的成年人的全国代表性样本中,他们参加了1988-1994年全国健康和营养调查III。根据LDL-C水平将受试者分为6组:<70、70–99.9、100–129.9、130–159.9、160–189.9和≥190mg/dL。通过与截至2015年12月31日的死亡记录的关联来确定死亡和潜在的死亡原因。加权Cox比例风险回归模型用于估计死亡率结果的风险比(HR)及其95%CI。
在304025人次每年的随访期间(中位随访时间23.2 年),发生了4458例死亡,其中1243例死于CVD。基线时,平均年龄为41.5岁,51.9%为女性。极低和极高水平的LDL-C与死亡率增加有关。在对年龄、性别、种族和民族、教育、社会经济地位、生活方式因素、C反应蛋白、体重指数和其他心血管危险因素进行调整后,与LDL-C<70mg/dL的个体相比LDL‐C为100–129.9mg/dL的受试者全因死亡率HRs为1.45(95%CI为1.10–1.93),CVD死亡HR为1.60(95%CI为1.01–2.54),卒中特异性死亡HR为4.04(95%CI为1.83–8.89),但没有增加冠心病死亡率的风险。
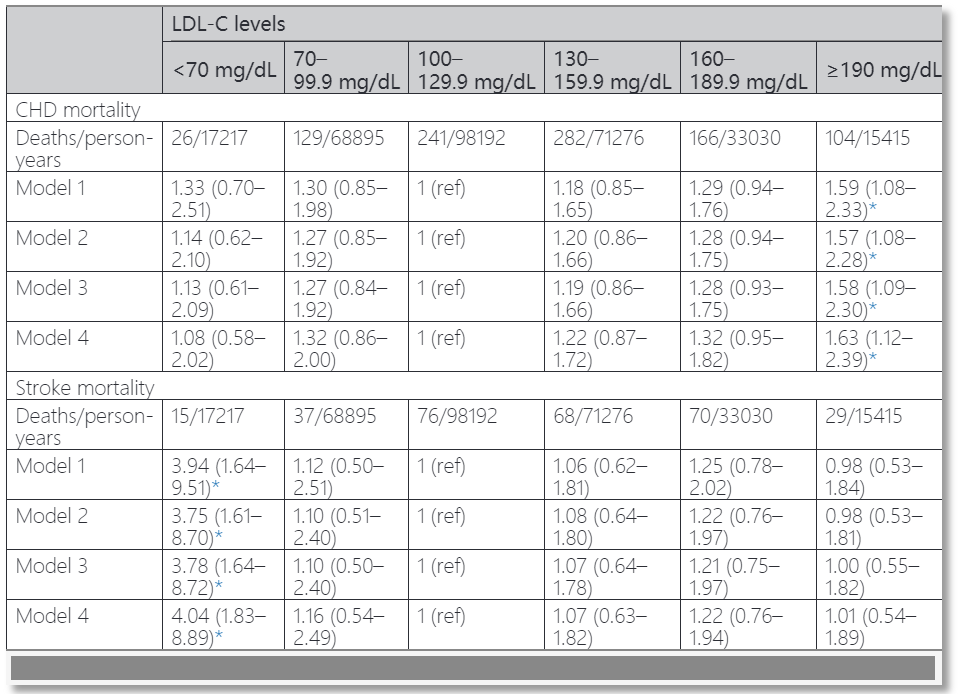
与LDL-C为100–129.9mg/dL的人相比,LDL-C≥190mg/dL的个体的心血管疾病死亡HR为1.49(95%CI为1.09–2.02),冠心病死亡HR为1.63(95%CI为1.12–2.39),但不会增加卒中死亡。
由此可见,非常低和非常高的LDL-C水平都与心血管疾病死亡风险增加有关。极低的LDL-C水平也与全因死亡率和卒中死亡的高风险相关。需要进一步调查以阐明一般人群中CVD健康的LDL-C水平的最佳范围。
原始出处:
Shuang Rong.et al.Association of Low‐Density Lipoprotein Cholesterol Levels with More than 20‐Year Risk of Cardiovascular and All‐Cause Mortality in the General Population.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.023690
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#全因死亡风险#
159 举报
任何事情都不能过度。
210 举报
#死亡风险#
112 举报
#AHA#
162 举报
#脂蛋白#
195 举报