哮喘新药显功效!tezepelumab将病情加重风险降低了56%
2021-02-27 Allan MedSci原创
TSLP靶向单克隆抗体tezepelumab已达到该试验的主要终点。
阿斯利康(AstraZeneca)和安进(Amgen)近日公布了III期NAVIGATOR研究的全部结果,研究结果表明,与安慰剂相比,在标准护理中加入tezepelumab可使重度、不受控制的哮喘患者的哮喘急性发作率(AAER)降低56%,且不论基线嗜酸性粒细胞计数如何。在两家公司去年11月宣布,TSLP靶向单克隆抗体tezepelumab已达到该试验的主要终点。
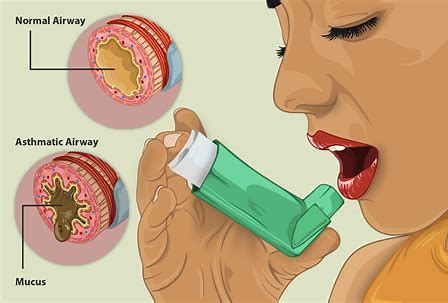
阿斯利康(AstraZeneca)生物制药研发部门负责人Mene Pangalos表示:“NAVIGATOR研究结果表明,tezepelumab能够显著减少哮喘急性发作频率。更为重要的是,无论患者基线嗜酸性粒细胞计数、过敏状态和呼出的一氧化氮(FeNO)如何,tezepelumab均有效”。
该试验招募了1059例12至80岁患有严重不受控制的哮喘患者,这些患者在52周内接受tezepelumab或安慰剂的皮下注射。在这些患者中,基线时血液嗜酸性粒细胞计数高和低的患者比例大致相等。
原始出处:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言


















#mAb#
77 举报
#风险降低#
84 举报
#病情加重#
97 举报
#PE#
73 举报
什么时候上市
91 举报
#病情#
80 举报
#Tezepelumab#
85 举报
#PEL#
85 举报