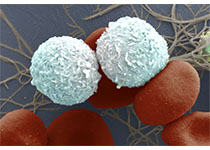
Oncotarget :三阴性乳腺癌新突破:科学家首次识别全新治疗靶点
2017-11-16 Heather_z727 来宝网
根据一项最新研究显示,研究人员找到了一种对激素治疗无效的致命乳腺癌机制,新的发现有望带来新的疗法和药物的开发。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#新突破#
84 举报
#target#
82 举报
#治疗靶点#
60 举报
#阴性乳腺癌#
67 举报
#三阴性#
76 举报