JAMA:冠状动脉旁路移植术 vs 经皮冠状动脉介入对高龄患者术后神经认知能力障碍风险的影响
2021-05-19 MedSci原创 MedSci原创
对于接受冠状动脉旁路移植术或经皮冠状动脉介入的高龄老年患者,患者术后记忆衰退率差异不显著

术后神经认知能力障碍(NCD)是老年患者常见的手术后并发症之一,而老年患者接受冠状动脉旁路移植术 (CABG)后NCD发病率尤其值得关注。2001年的观察性研究称,CABG后5年,42%的患者认知能力下降明显。有研究称,体外循环冠状动脉旁路移植术与不良神经功能结果相关,但这一结论尚未得到证实。近日研究人员比较了老年患者接受冠状动脉旁路移植术或经皮冠状动脉介入治疗(PCI)后记忆减退率的变化。
本次研究为对退休社区居民的回顾性队列研究,参与者于1998-2015年间接受了CABG(体外循或非体外循)或PCI,参与者手术年龄在65岁以上。研究的主要终点为每2年1次的记忆分数变化。
1680名参与者,平均手术年龄为75岁,41%为女性,665人接受CABG(168例非体外循CABG),1015例接受PCI。PCI组术前平均记忆减退率为0.064记忆单位/年,术后平均记忆减退率为0.060记忆单位/年(组内变化为0.004记忆单位/年)。CABG组,术前平均记忆减退率为0.049记忆单位/年,术后平均记忆减退率为0.059记忆单位/年(组内变化为-0.011记忆单位/年)。PCI组与CABG组记忆减退率差异为0.015记忆单位/年,无显著性差异。进一步的区分CABG类型后发现,与PCI术后相比,非体外循环CABG后,记忆减退程度加大,差异为0.046记忆单位/年,但与PCI相比,体外循环CABG后,记忆减退程度不明显,差异为0.003记忆单位/年。
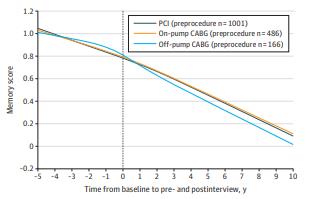
PCI vs CABG组患者记忆得分变化
研究认为,对于接受冠状动脉旁路移植术或经皮冠状动脉介入治疗的高龄老年患者,患者术后记忆衰退率差异不显著。
原始出处
Elizabeth L. Whitlock et al. Association of Coronary Artery Bypass Grafting vs Percutaneous Coronary Intervention With Memory Decline in Older Adults Undergoing Coronary Revascularization.JAMA. May 18, 2021.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#旁路移植术#
0 举报
#高龄患者#
114 举报
#移植术#
134 举报
#冠状动脉旁路移植术#
147 举报
#高龄#
115 举报
#神经认知#
135 举报
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
99 举报
最新威廉亚洲官网 ?
93 举报