NEJM里程碑式定论:高血压患者收缩压<120mmHg可显著降低心血管死亡率!
2021-05-22 MedSci原创 MedSci原创
积极的血压管理大大降低了心脏病、中风和这些疾病的死亡风险,以及所有原因导致的死亡。
随着医学进步,高血压阈值和关于高血压的主流观念已经发生变化。关于单纯舒张期高血压单纯收缩期高血压及联合收缩期和舒张期高血压所导致的后果,20世纪60年代出现了相关概念,当时流行的观点是只有舒张期高血压影响结局。
弗雷明汉(Framingham)心脏研究和其他研究表明,收缩期高血压作为心血管结局的预测因素,其重要性实际上超过舒张期高血压,因此有人呼吁“不再关注舒张压”。因此美国心脏病学会/美国心脏学会(ACC/AHA)风险估计工具在确定心血管风险时也未考虑舒张压。
然而,去年发表在《新英格兰医学杂志》(NEJM)杂志上的一项重磅研究则为舒张压进行了“正名”。研究对超过100万人、3600万次的血压测量数据显示,“上压”、“下压”都是心梗或中风发作风险的独立预测因素。2018年欧洲心脏病学会(ESC)高血压威廉亚洲博彩公司 也建议所有风险水平患者的最佳舒张压目标为70至80 mmHg。
近日,NEJM再次发表了具有里程碑意义的高血压对心血管疾病影响(SPRINT研究的后续数据,证实,积极的血压管理--将收缩压降低到120mmHg以下--与将收缩压降低到140mmHg以下相比,大大降低了心脏病、中风和这些疾病的死亡风险,以及所有原因导致的死亡。
SPRINT是一项随机对照的临床试验,由美国国家卫生研究院(NIH)下属的国家心肺和血液研究所赞助。此前SPRINT试验也曾公布过相关结果,阿拉巴马大学伯明翰分校公共卫生学院流行病学系教授兼主任、该研究的主要调查员Cora E. Lewis博士说:"对最初的SPRINT研究结果的一个批评是,在主要结果的各个组成部分中,只有心力衰竭和心血管疾病导致的死亡在强化治疗组中明显降低。但此次最终结果发现,心脏病发作的风险,以及心力衰竭和心血管疾病死亡的风险,在治疗量低于120的组别中明显降低,而在更密集治疗的组别中,不包括心力衰竭的主要结果的风险仍然明显降低。"
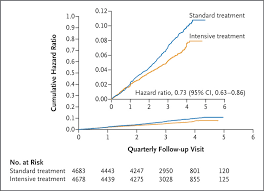
随访期间,强化治疗组(蓝)与标准治疗组(黄)主要结局事件发生率
研究人员随机分配了9361名心血管疾病风险增加但没有糖尿病或既往中风的参与者进行强化治疗(收缩压<120mmHg)或标准治疗(收缩压<140mmHg)。研究主要结果是心肌梗死、其他急性冠状动脉综合征、中风、急性失代偿性心力衰竭或心血管原因导致的死亡。
在中位数为3.33年的随访中,强化治疗组的主要结果和全因死亡率明显低于标准治疗组(主要结果比率:1. 77%/年 vs 2.40%/年,OR=0.73;全因死亡率: 1.06%/年vs 1.41%/年,OR=0.75),分别降低27%与25%。
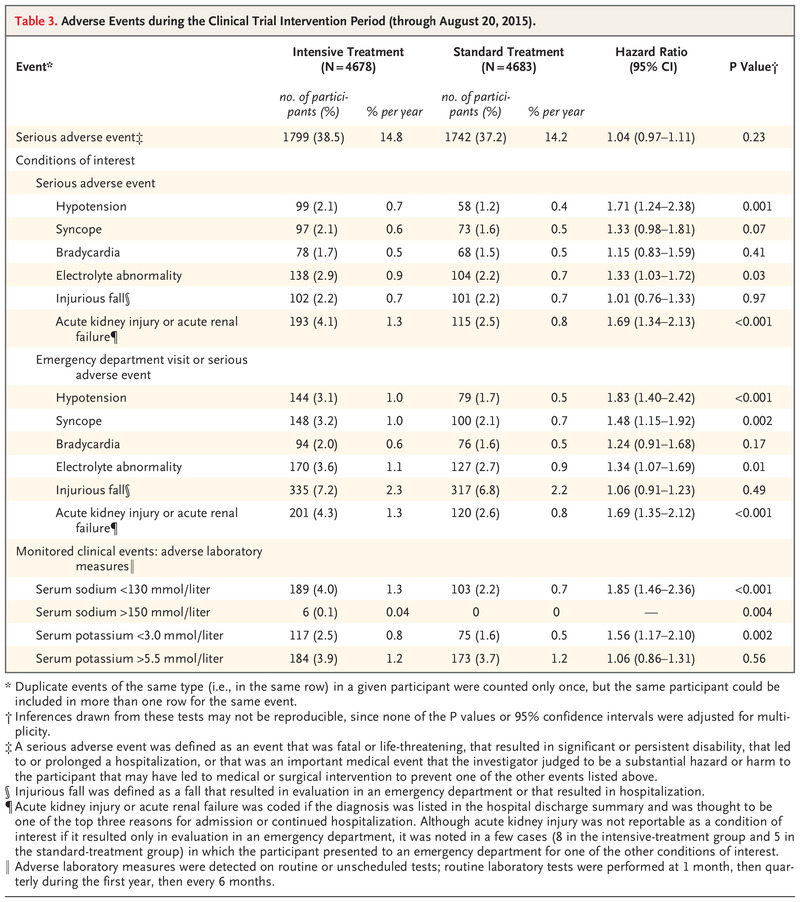
两组治疗相关不良事件的发生率
进一步在排除非致死性心衰后,强化降压治疗仍能降低28%心梗、37%心衰和42%心血管原因死亡率。亚组分析同样支持了强化降压治疗的获益。
同时,虽然低血压、电解质异常、急性肾损伤或衰竭以及晕厥等严重不良事件在强化治疗组明显更频繁,但两组的严重不良事件发生率没有显著差异。
综上,对于高血压人群,强化血压管理、收缩压低于120 mmHg可以显著降低心脏病、中风和死亡风险。
参考文献:
Final Report of a Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med 2021; 384:1921-1930. DOI: 10.1056/NEJMoa1901281
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言















#里程碑#
91 举报
#收缩压#
84 举报
高血压隐形杀手
101 举报
#心血管死亡率#
134 举报
#高血压患者#
0 举报
#心血管死亡#
84 举报
高血压预防病发症
161 举报
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
83 举报
好文章!
106 举报