不可手术腱鞘巨细胞瘤患者的福音!国内首个靶向创新药获突破性疗法认定
2022-07-26 生物探索 生物探索
对于腱鞘巨细胞瘤,手术切除是长期以来的经典治疗手段,然而实际操作中,部分患者手术切除难度大,或者手术风险非常高。
“对于腱鞘巨细胞瘤(tenosynovial giant cell tumor,TGCT),手术切除是长期以来的经典治疗手段,然而实际操作中,部分患者手术切除难度大,或者手术风险非常高。靶向药物的出现给了不能手术的腱鞘巨细胞瘤患者一个新的治疗选择。”北京积水潭医院骨肿瘤科主任牛晓辉教授在接受采访时表示。
而牛晓辉教授提到的靶向创新药,正是港股创新药企和誉医药自主研发的高选择性CSF-1R抑制剂ABSK021。近日,该药物被中国国家药品监督管理局药品审评中心(CDE)认定为突破性治疗药物,用于治疗不可手术的腱鞘巨细胞瘤,这也是首个由中国公司独立自主研发并推进临床的高选择性CSF-1R抑制剂。
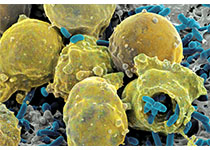
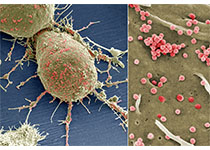
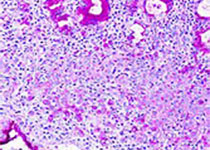
根据公开信息,腱鞘巨细胞瘤是一种罕见的局部浸润性软组织肿瘤,主要因过表达集落刺激因子-1(CSF1)引起,最常见于关节滑膜、滑囊或腱鞘,临床表现为受累关节疼痛和僵硬、肿胀、出血性关节积液、关节周围糜烂、软骨退化和继发性骨关节炎,严重影响患者生活质量。
“腱鞘巨细胞瘤的发病率每百万人约有43人患病,属于罕见病。该病可分为弥漫性和局限性两种,其中局限性患病人数约为弥漫性的近10倍。”牛晓辉教授表示,“而且这一疾病多发于青中年,病史较长,早期可能没有明显的症状,容易被误诊。”
在诊疗维度,手术切除是腱鞘巨细胞瘤长期以来的经典治疗手段,但部分患者由于切除难度大,可能涉及全滑膜切除、关节置换甚至截肢,手术并发症风险也较高,并不适合手术切除。另外,有文献报道超过50%的弥漫性腱鞘巨细胞瘤患者手术切除后仍出现复发。
“有的患者来就诊时肿瘤已经非常大了,而且腱鞘巨细胞瘤仿佛‘寄生’在正常组织内,在切除肿瘤的时候,会不可避免的伤害到正常组织,此时手术风险就非常高,可能涉及全滑膜切除、关节置换甚至截肢。”牛晓辉教授说,“患者服用ABSK021后,williamhill asia 可以明显的感觉到患者肿瘤的缩小。”
值得注意的是,目前国内尚无针对无法手术的腱鞘巨细胞瘤患者的治疗药物上市,因此本次ABSK021纳入突破性疗法的认定,有望加速该药物的关键临床研究和上市,为患者带来全新的治疗选择。
据悉,突破性疗法认证是CDE对创新药物审评的四种加快程序之一,有严格的认定标准。在药物临床试验期间,用于防治严重危及生命或者严重影响生存质量的疾病,且尚无有效防治手段或者与现有治疗手段相比有充分证据表明具有明显临床优势的创新药或改良型新药,可申请CDE突破性治疗药物程序。ABSK021获得突破性疗法认定是基于临床Ib期试验在腱鞘巨细胞瘤患者中的优异研究结果。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#腱鞘巨细胞瘤#
82
#创新#
92
#细胞瘤#
104
#巨细胞#
88
#突破性疗法#
92
认真学习~~
88